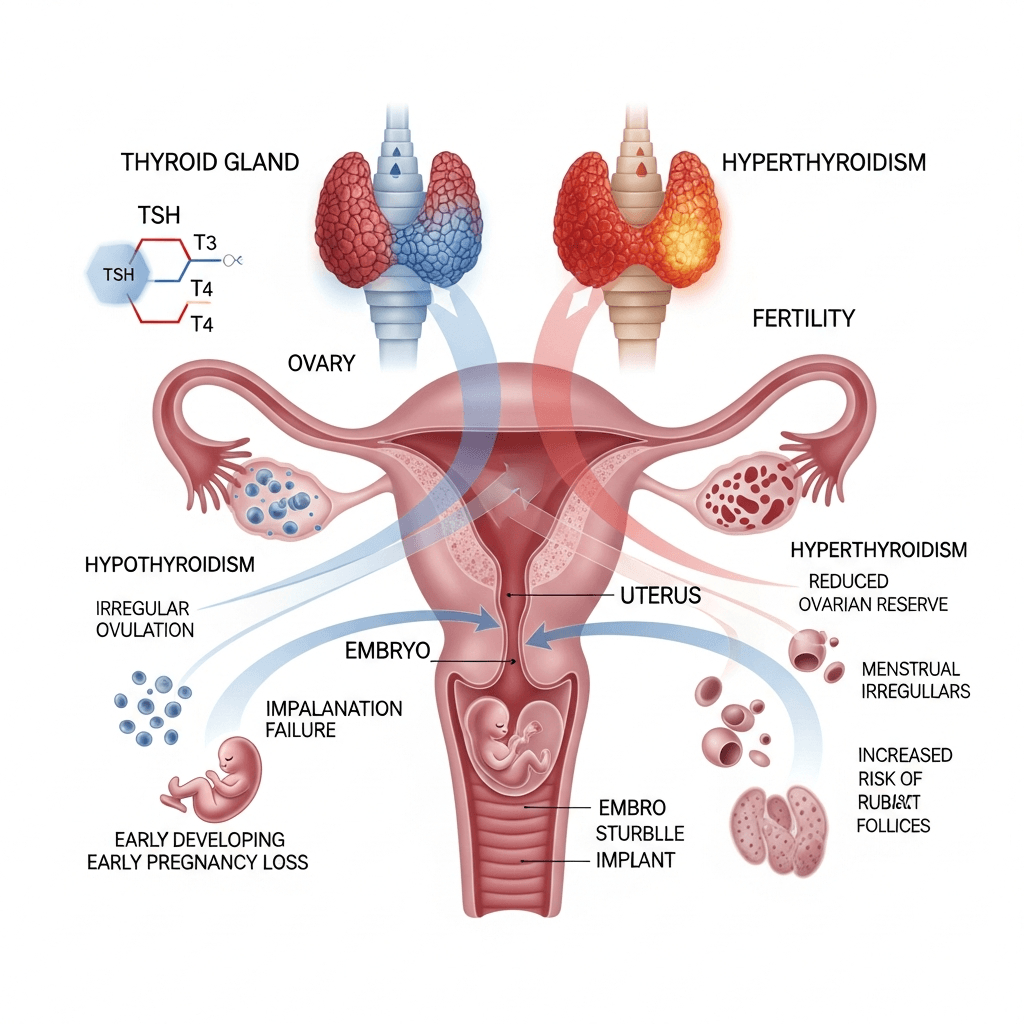
Thyroid health plays a far more important role in fertility than most people realize. Whether you are trying to conceive naturally or preparing for an IVF cycle, keeping your thyroid hormones in balance is crucial. Even a slight imbalance in thyroid function—either hypothyroidism (low thyroid hormone) or hyperthyroidism (excess thyroid hormone)—can interfere with ovulation, menstrual regularity, embryo implantation, and overall IVF success rates.
Many couples struggling with infertility later discover that an undiagnosed thyroid problem may have been affecting their chances of conception. That is why leading fertility specialists emphasize complete thyroid screening before starting assisted reproductive treatments. If you are searching for guidance or planning IVF, consulting the best IVF doctor in Delhi or your region can help ensure that your thyroid levels are well-controlled before treatment begins.
This blog explains how thyroid disorders impact fertility, IVF outcomes, pregnancy, and what steps you can take to improve your reproductive health.
Understanding the Thyroid’s Role in Fertility
The thyroid gland produces hormones that regulate metabolism, energy levels, menstrual cycles, and reproductive hormones. Even small fluctuations in thyroid hormones—T3, T4, and TSH—can impact:
- Ovulation
- Menstrual regularity
- Ovarian response to stimulation
- Embryo quality
- Endometrial receptivity
- Successful implantation
- Maintaining a healthy pregnancy
A healthy thyroid ensures a stable hormonal environment, which is essential for both natural conception and IVF success.
Types of Thyroid Disorders That Affect Fertility
1. Hypothyroidism (Underactive Thyroid)
Hypothyroidism is one of the most common thyroid conditions in women seeking fertility treatment. Low thyroid hormone levels cause:
- Irregular or missed periods
- Anovulation (lack of ovulation)
- High prolactin levels, which further suppress ovulation
- Poor quality of eggs
- Luteal phase defects
- Lower implantation rates
Women with untreated hypothyroidism often face difficulties conceiving naturally, and the condition can significantly reduce IVF success rates if not managed properly.
2. Hyperthyroidism (Overactive Thyroid)
Hyperthyroidism is less common but equally troublesome for fertility. Excess thyroid hormone may lead to:
- Short or light menstrual cycles
- Premature ovarian failure
- Miscarriages
- Poor embryo implantation
- Pregnancy complications
If you have symptoms like weight loss, rapid heartbeat, or heat intolerance, it’s essential to get your thyroid evaluated before starting IVF.
3. Autoimmune Thyroid Disorders (Hashimoto’s, Graves’ Disease)
Thyroid autoimmunity plays a silent yet powerful role in fertility challenges. Thyroid antibodies such as TPO (thyroid peroxidase) and TG (thyroglobulin) can negatively affect:
- Egg quality
- Embryo development
- Implantation success
- Fresh and frozen embryo transfer outcomes
Studies show that even when TSH levels are normal, women with thyroid antibodies experience lower IVF success rates. This is why many specialists—especially the best IVF doctors in Delhi—recommend antibody testing as part of pre-IVF evaluation.
How Thyroid Disorders Impact IVF Success Rates
1. Affecting Ovarian Stimulation Response
Women with thyroid imbalances may respond poorly to ovarian stimulation medications. This can result in fewer mature eggs and lower fertilization potential during IVF.
2. Lower Embryo Quality
Thyroid hormones influence cellular growth. Abnormal levels may affect egg maturation and embryo development, leading to weaker embryos that are less likely to implant.
3. Implantation Failure
The endometrium must be hormonally synchronized for implantation. Thyroid dysfunction disrupts the endometrial lining, making it less receptive to the embryo.
4. Increased Risk of Miscarriage
Even after a successful implantation, thyroid disorders—especially autoimmune thyroiditis—can increase the risk of early pregnancy loss.
5. Disturbance in Hormonal Balance
Thyroid disorders often disrupt other hormones such as prolactin, estrogen, and progesterone, all of which are essential for a successful IVF cycle.
The Ideal Thyroid Levels Before IVF
Fertility experts generally recommend:
- TSH level between 1.0 – 2.5 mIU/L (optimal for conception and early pregnancy)
- T3 and T4 within the normal range
- Negative or low thyroid antibodies, if possible
- Stable levels for at least 6–8 weeks before starting IVF
Maintaining these levels improves ovarian response, embryo quality, and implantation rates.
If your thyroid levels are not optimal, a fertility specialist will customize treatment before starting IVF protocols.
How Thyroid Disorders Are Diagnosed During IVF Evaluation
A comprehensive fertility assessment usually includes:
- TSH (Thyroid-Stimulating Hormone)
- Free T3
- Free T4
- Anti-TPO antibodies
- Anti-TG antibodies
For patients at risk or with symptoms, additional tests may be recommended.
Treatments to Enhance IVF Success in Thyroid Patients
1. Medication and Hormone Replacement
- Hypothyroidism is treated with Levothyroxine
- Hyperthyroidism may require anti-thyroid medications
Consistent monitoring ensures stable levels before embryo transfer.
2. Antibody Management
For autoimmune thyroid issues, doctors may prescribe:
- Low-dose steroids
- Selenium supplements
- Lifestyle modifications
- Anti-inflammatory diet
3. Lifestyle Changes
Healthy habits support thyroid balance:
- Adequate sleep
- Stress reduction
- Avoiding excessive iodine
- Regular exercise
- Balanced meals rich in selenium, zinc, and B vitamins
4. Close Monitoring During IVF Cycle
You may need thyroid function tests every 4–6 weeks, especially after starting hormonal stimulation.
Thyroid Disorders and Pregnancy After IVF
Even after a successful IVF cycle, thyroid levels must be monitored closely. Poor thyroid control during pregnancy can lead to:
- Preterm birth
- Low birth weight
- Preeclampsia
- Developmental issues in the baby
- Pregnancy loss
This is why many couples prefer consulting experienced specialists such as the best IVF doctors in Delhi, who have extensive experience managing complex cases like infertility linked with thyroid disorders.
When Should You See a Fertility Specialist?
You should consult a fertility expert if you:
- Have irregular periods
- Have been diagnosed with thyroid disease
- Are over 35
- Are planning IVF
- Have had multiple miscarriages
- Experience symptoms of thyroid imbalance
A specialist will design a personalized treatment plan that addresses both fertility and thyroid health.
Final Thoughts
Thyroid health is deeply connected to reproductive wellbeing. Whether you’re trying naturally or preparing for IVF, addressing thyroid issues early can significantly improve your chances of conceiving and maintaining a healthy pregnancy. With the right diagnosis, treatment, and medical guidance, many women with thyroid disorders successfully achieve pregnancy through IVF.