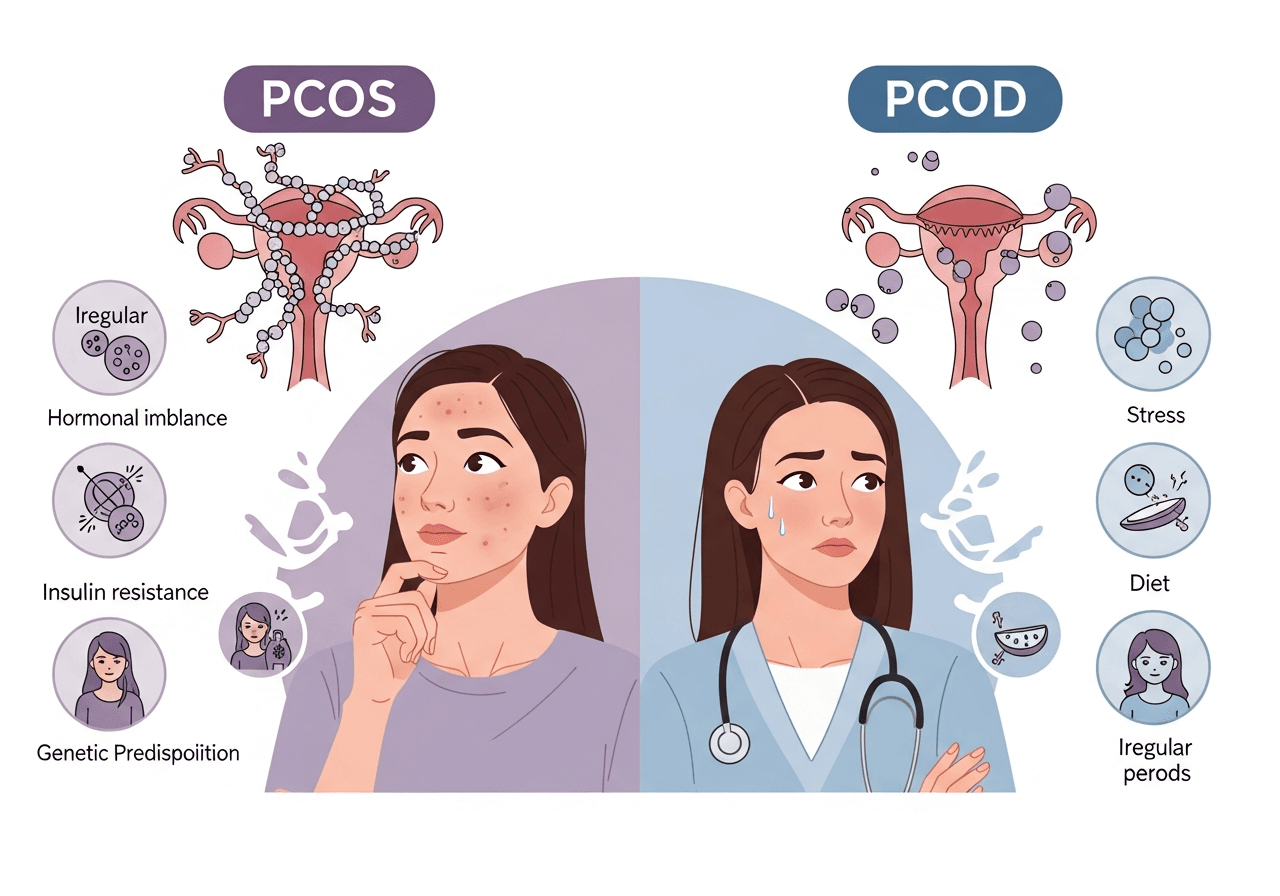
Why is your menstrual cycle playing hide and seek, or why is an unexplainable gain in weight gain ruining your workout plans? PCOS is often not differentiated from PCOD; however, understanding their difference can help thousands of women take control of their reproductive health.
Defining PCOS and PCOD
Polycystic Ovary Syndrome (PCOS) is a common endocrine system disorder that occurs in 5-10 percent of women at reproductive age, and hormonal disorders, insulin resistance, and small cysts on the ovaries also characterize it.
Polycystic Ovarian Disease (PCOD) is thought to be milder in nature, where the ovaries are unable to release mature eggs regularly, which causes the formation of cysts due to hormonal imbalances.
Even though PCOS and PCOD exhibit similarities and show ovarian cysts on an ultrasound, metabolism is affected everywhere on the bodies of individuals affected by PCOS, thus increasing the risks of developing diabetes and heart disease, unlike PCOD, which mainly affects menstrual patterns.
Key Differences
PCOS and PCOD overlap in symptoms but diverge in severity and scope. Think of PCOD as a local ovarian glitch, PCOS as a full-body hormonal storm.
| Aspect | PCOD | PCOS |
| Nature | Hormonal imbalance in the ovaries / Ovarian dysfunction | Endocrine/metabolic syndrome |
| Severity | Mild, reversible with lifestyle | Severe, chronic |
| Androgens | Slight increase | High levels causing hirsutism/acne |
| Periods | Irregular | Often absent |
| Fertility | Manageable naturally | Often requires infertility treatment |
| Complications | Limited to the ovaries | Insulin resistance, obesity, diabetes |
| Prevalence | More common (up to 20%) | Less common but serious |
| Cysts | Multiple, functional | Polycystic morphology |
These distinctions guide diagnosis via blood tests, ultrasounds, and clinical history.
Common Causes
PCOS and PCOD are both similar in terms of their common predisposing factors, which include genetic factors, hormonal imbalances, insulin resistance, and lifestyle factors, but PCOS shows a majority of systemic metabolic abnormalities.
Key Causes
Both conditions cause ovarian androgen production that results from elevated levels of insulin in the body, typically because of insulin resistance, and disrupted ovulation and follicle maturation, which is more severe in PCOS.
Heredity plays a role in this as well:
A family history of PCOD or PCOS, especially in close relatives such as your mother or sister, may indicate you have a high chance of developing it as well.
Lifestyle and Inflammation Factors
Poor diet, sedentary lifestyles, chronic stress, obesity, and irregular sleep, among other factors that play a significant role, especially in PCOD, as they worsen hormonal imbalance and the development of cysts due to immature eggs.
The consequences of low-grade chronic inflammation associated with oxidative stress and agentic cytokines such as TNF-α include the aggravation of insulin resistance and hyperandrogenism, particularly in PCOS. These are factors that can be changed, which is why early action matters.
Emerging research links exposure to per- and polyfluoroalkyl substances (PFAS), known as “forever chemicals” found in non-stick cookware, water-resistant fabrics, and contaminated water, with increased PCOS risk. (1)
Overlapping Symptoms
The symptoms are indistinct, but the severity differs.
- Irregular or absent periods affect 70-80% of women in both cases, with weight gain and bloating.
- The other common symptoms are acne, excessive facial and/or body hair (hirsutism), loss of hair, and infertility as a result of anovulation.
- PCOS symptoms such as fatigue, mood swings, and skin darkening (acanthosis nigricans) are primarily caused by the underlying hormonal imbalances and insulin resistance. (2)
Diagnosis Essentials
A single test can confirm neither PCOS nor PCOD. However, there are still diagnoses that are essential and need expert intervention.
PCOS Diagnosis
PCOS follows the Rotterdam criteria: oligo-ovulation or anovulation (irregular/infrequent periods), clinical/biochemical hyperandrogenism (hirsutism, acne, elevated testosterone), and polycystic ovarian morphology on ultrasound (≥12 follicles 2-9 mm per ovary or ovarian volume >10 mL) after ruling out mimics. (3)
PCOD Diagnosis
PCOD lacks formal criteria but is diagnosed clinically via menstrual irregularities, ultrasound showing multiple small follicular cysts (typically >10 per ovary), and absence of full PCOS metabolic features like severe insulin resistance or marked hyperandrogenism; blood tests assess LH/FSH ratio (often >2:1 in PCOS/PCOD), testosterone, and insulin resistance.
Early diagnosis will avoid complications such as endometrial hyperplasia.
Treatment Approaches
Lifestyle is the most important: weight reduction (lose 5-10% body weight) using balanced diets (low in glycemic index, high fiber/protein), daily 30 minutes exercise, stress reduction using yoga/meditation.
PCOD usually cures itself; PCOS requires drugs, such as metformin to maintain insulin levels, combined hormones during menstrual periods, or anti-testosterone to treat hirsutism.
When ovulation induction is needed, such as clomiphene is used to aid fertility in PCOD, however, more advanced treatments may be required in PCOS.
Infertility treatment in Delhi centers is the best, providing personalized treatment plans like scheduling an appointment with an IVF doctor in Delhi in intractable cases. Surgery (laparoscopic drilling of the ovary) is a rare case as a last resort.
Fertility and Long-Term Management
Infertility hits hard, and with PCOD, it is possible to conceive after some lifestyle changes, although PCOS is associated with 70 percent anovulatory infertility, and it may require IVF. Consult an IVF doctor in Delhi when one has tried for more than a year, and nothing has come up. The clinics offer hormone checks and embryo services. In the long term, watch for type 2 diabetes (half of the people at risk of PCOS), heart problems, and mental trouble -his/her screenings should be performed annually.
Living Well with PCOS/PCOD
Get Stronger: Monitor loops using applications, make sleep a priority, and create a mental health network. Anti-inflammatory foods suggested by nutritionists are berries, nuts, and greens. When symptoms are persistent, it is advisable to seek professional advice on a case-by-case basis- lots of them can survive after the management. It is important to keep in mind that the initial step to hormonal harmony is knowledge.
If you are looking for effective PCOS and PCOD treatment in Delhi, it is essential to consult an experienced specialist for accurate diagnosis and long-term management. Dr. Sowjanya Aggarwal, a leading gynecologist and PCOS/PCOD specialist in East Delhi and Ghaziabad, provides comprehensive and personalized care for women suffering from polycystic ovary syndrome (PCOS) and polycystic ovarian disease (PCOD). At her clinic FEMMENEST, patients receive advanced PCOS treatment, including hormonal evaluation, menstrual cycle regulation, lifestyle and diet guidance, fertility support, and individualized medical care. With a strong focus on evidence-based treatment, Dr. Sowjanya Aggarwal helps women manage PCOS symptoms, improve reproductive health, and enhance overall well-being. Visit Dr. Sowjanya Aggarwal’s clinic in East Delhi / Ghaziabad to consult a trusted expert for PCOS and PCOD treatment near you.